B vitamins can potentially be used to treat advanced non-alcoholic fatty liver disease
A mechanism that causes an advanced type of fatty liver disease has been discovered by researchers at Duke-NUS Medical School in Singapore; it turns out that vitamin B12 and folic acid supplements can stop this mechanism.
These results might benefit those who suffer from non-alcoholic fatty liver disease, which is a catch-all phrase for a variety of liver disorders affecting people who consume little to no alcohol and which affects 4 in 10 adults in Singapore and 25% of all adults worldwide.
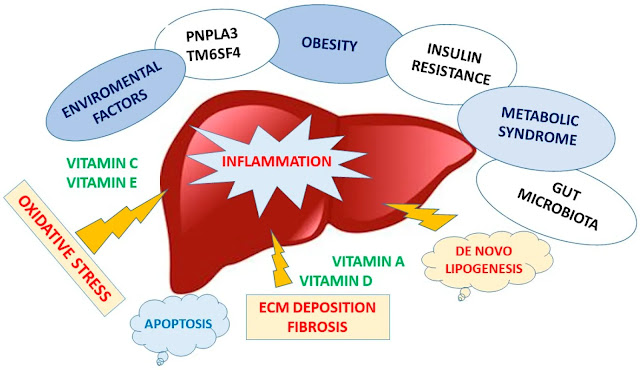
The most common reason for liver transplants globally is non-alcoholic fatty liver disease, which causes fat to accumulate in the liver. Due to its link to diabetes and obesity, two serious public health issues in Singapore and other developed nations, it has a high prevalence. Non-alcoholic steatohepatitis is the term used when the disorder proceeds to inflammation and the production of scar tissue (NASH).
The study's first author, Dr. Madhulika Tripathi, a senior research fellow with the Laboratory of Hormonal Regulation at Duke-NUS' Cardiovascular & Metabolic Programme, said that while liver fat deposition is reversible in its early stages, its progression to NASH causes liver dysfunction, cirrhosis, and raises the risk for liver cancer.
NASH has no pharmaceutical therapy at this time since researchers don't fully comprehend how the illness works. The significance of homocysteine in the development of NASH remains unknown, despite the fact that it is known that the illness is linked to high blood levels of this amino acid.
The relationship between homocysteine and the development of NASH in preclinical models and people was validated by Dr. Tripathi, research co-author Dr. Brijesh Singh, and their associates in Singapore, India, China, and the US. Additionally, they discovered that when homocysteine concentrations in the liver rose, the amino acid linked to different liver proteins, altering their composition and impairing their functionality. Homocysteine specifically prevented a protein known as syntaxin 17 from carrying and digesting fat (known as autophagy, an important cellular process by which cells eliminate misfolded proteins or damaged organelles) in fatty acid metabolism, mitochondrial turnover, and the suppression of inflammation. This caused NASH to develop and progress from fatty liver disease.
Importantly, the researchers discovered that adding vitamin B12 and folic acid to the preclinical animals' diets raised the levels of syntaxin 17 in the liver and restored its function in autophagy. Additionally, it stopped the progression of NASH and treated liver fibrosis and inflammation.
Because they imply that a reasonably cheap medication, vitamin B12 and folic acid, might be used to stop or postpone the advancement of NASH, Dr. Singh noted that his team's results are both fascinating and significant. Homocysteine levels in the liver and serum might also be used as a biomarker to gauge the severity of NASH.
Finding out whether liver proteins may also be impacted similarly by homocysteine is one of the team's next research priorities. They anticipate that more study will result in the creation of anti-NASH treatments.
The potential use of vitamin B12 and folate, which have high safety profiles and are classified as dietary supplements by the US Food and Drug Administration, as first-line therapies for the prevention and treatment of NASH could result in significant cost savings and lessen the health burden from NASH, according to Professor Paul M. Yen, Head of the Laboratory of Hormonal Regulation at Duke-NUS' Cardiovascular & Metabolic Disorders Program and senior author of the study.
Senior Vice-Dean for Research at Duke-NUS, Professor Patrick Casey, stated: "Currently, a liver transplant is the sole option for individuals with end-stage liver disease. The research by Dr. Tripathi and her associates shows that a straightforward, reasonably priced, and easily available intervention may be able to stop or cure liver damage, giving patients who have fatty liver illnesses fresh hope. The team's findings highlight the importance of fundamental scientific research, which enables the scientific community to continue having a significant beneficial influence on patients' lives."
Story Source:
Materials provided by Duke-NUS Medical School. Note: Content may be edited for style and length.



Comments
Post a Comment